People with HIV who were treated with the antiretrovirals Retrovir (zidovudine, or AZT) or Videx (didanosine, or ddI) have a greater risk of liver damage, although hepatitis C virus (HCV) coinfection is associated with the greatest elevated risk of this health outcome, aidsmap reports. Fully suppressing HIV with ARVs is, however, associated with a 50 percent reduction in such risk.
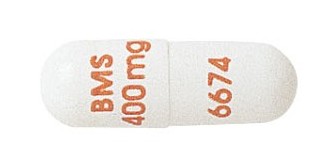
Retrovir and Videx were among the first available ARVs and are associated with numerous toxicities. They are not commonly prescribed to treat HIV today.
Publishing their findings in PLOS ONE, researchers conducted a cross-sectional study of 333 adults who received medical care for HIV between 2009 and 2011.
The cohort had a median age of 45. Eighty-three percent were male. About one in four had contracted HIV through injection drug use or infected blood products. Eighty-nine percent were taking ARVs, for a median of five years. One in three were coinfected with HCV, and 7 percent were coinfected with HBV. One third had taken AZT in the past, and 12 percent had taken Videx.
Eighteen percent of the cohort had significant fibrosis, or scarring, of the liver, while 8 percent had cirrhosis, which is a stage of liver disease more severe than advanced fibrosis. The rates of each liver condition were higher among those coinfected with HCV compared with those who only had HIV.
After adjusting the data for various factors, the researchers found that factors associated with an increased risk of significant fibrosis included HCV coinfection (5.3-fold increased risk) and having taken Videx (2.7-fold increased risk). Having a fully suppressed HIV viral load was associated with a 50 percent reduced risk of significant fibrosis. Factors associated with an increased risk of cirrhosis included HCV coinfection (5.8-fold increased risk), having taken Videx (2.9-fold increased risk) and having taken Retrovir (2.8-fold increased risk).
Among those who had only HIV and not HCV, having a fully suppressed viral load was associated with a 60 percent reduced risk of having significant fibrosis, while having taken Videx was associated with a 20.8-fold increased risk of cirrhosis.
“In conclusion,” the study authors wrote, “history of exposure to [Videx] and [Retrovir] continues to have an impact on the presence of liver cirrhosis in HIV patients. However, HCV coinfection and ongoing HIV-replication have the strongest effect on development of significant fibrosis in these patients.”
To read the study, click here.
To read the aidsmap article, click here.






Comments
Comments